The Centers for Medicare and Medicaid Services (CMS) is planning to release shadow bundles data to ACO participants (including those participating in the MSSP and ACO REACH models) to provide increased transparency into hospital and specialty care. Results of a CMS poll1 indicated “95% of ACO respondents were likely or very likely to utilize shadow bundles data to support better specialty engagement.” This paper outlines information ACOs in the MSSP and ACO REACH models will receive when this data is released in early 2024, how it can be used, and other considerations in using provider performance benchmarking data to better manage specialty care.
What are shadow bundles?
Shadow bundles are a type of bundled payment that is built within an ACO’s attributed population. A bundled payment is a fixed-price agreement for a predefined episode of care, commonly consisting of a procedure and all related services or all care for a medical condition.2 While bundled payments traditionally come with fixed-price agreements for the agreed services, CMS is currently providing shadow bundles to MSSP and ACO REACH participants for informational purposes only.
For these shadow bundles, CMS will leverage a modified version of the Bundled Payment for Care Improvement – Advanced (BPCI-A) program of the Center for Medicare and Medicaid Innovation (CMMI) bundled payment episode methodology. BPCI-A episodes capture care related to 29 inpatient, three outpatient, and two multi-setting clinical episodes that span cardiac, pulmonary, gastrointestinal, spine, bone and joint, kidney, infectious disease, and neurology conditions. The scope of BPCI-A episodes covered roughly 23% of total Medicare Parts A and B expenditures as observed in CMS’s 100% Medicare Fee-for-Service (FFS) dataset in calendar year (CY) 2021.
BPCI-A episode definitions include the beneficiary’s total cost of care (with some minor exclusions) beginning at the start of the admission or surgery (i.e., the triggering event) and extending 90 days post-discharge or -surgery (or until death). Because BPCI-A episodes can be aggregated based on the triggering event or the care that happens in the 90 days following the triggering event, they can be leveraged in a variety of ways to better understand and manage beneficiary care, including provider profiling, post-acute facility profiling, and performance benchmarking.
What shadow bundle data will MSSP AND ACO REACH participants receive?
The shadow bundles data being shared with ACOs in the MSSP and ACO REACH models is informational only and will not impact shared savings. Model participants will receive three types of data files with varying frequency and detail:
- Monthly episode-level files: Monthly episode and claims-level files for all shadow bundles initiated by the ACOs attributed beneficiaries.
- Quarterly summary reports: Quarterly summary files of the monthly claims and episode data files that are intended to require no data manipulation from the user.
- Annual benchmark prices: Annual summary report with prospective benchmark prices by clinical episode, with adjustments for the reporting year’s payment rates.
How can MSSP and ACO REACH participants leverage this shadow bundles data?
The shadow bundles data CMS will be providing will give ACOs insight into hospital and individual specialist performance. This data can be very powerful when ACOs consider strategies around referrals and partnerships with hospitals and specialists and identify areas of cost improvement to reduce the total cost of care of their attributed populations. The following are ways ACOs may be able to best leverage this data.
Develop post-acute care (PAC) strategies to improve overall total cost of care and outcomes
Shadow bundles create episodes of care that enable insights not only on the care provided during a hospital admission or surgery, but also on the larger patient journey post-discharge or -surgery. By evaluating performance or expenditures within the context of an episode, more targeted and actionable areas of opportunity can be identified to improve performance. Benchmarking across various components of episodes, such as the post-acute care (PAC) setting, clinical episode, or hospital, will enable ACOs to understand how their episodic spend compares to others in a variety of ways. This helps ACOs better understand if and where opportunities for improvement may exist. If shadow bundle data indicates an ACO has higher PAC utilization compared to benchmarks, potential remediation may include directing care management resources toward better managing PAC utilization or structuring a risk contract with one or all of the organizations that provide care that falls within a given clinical episode.
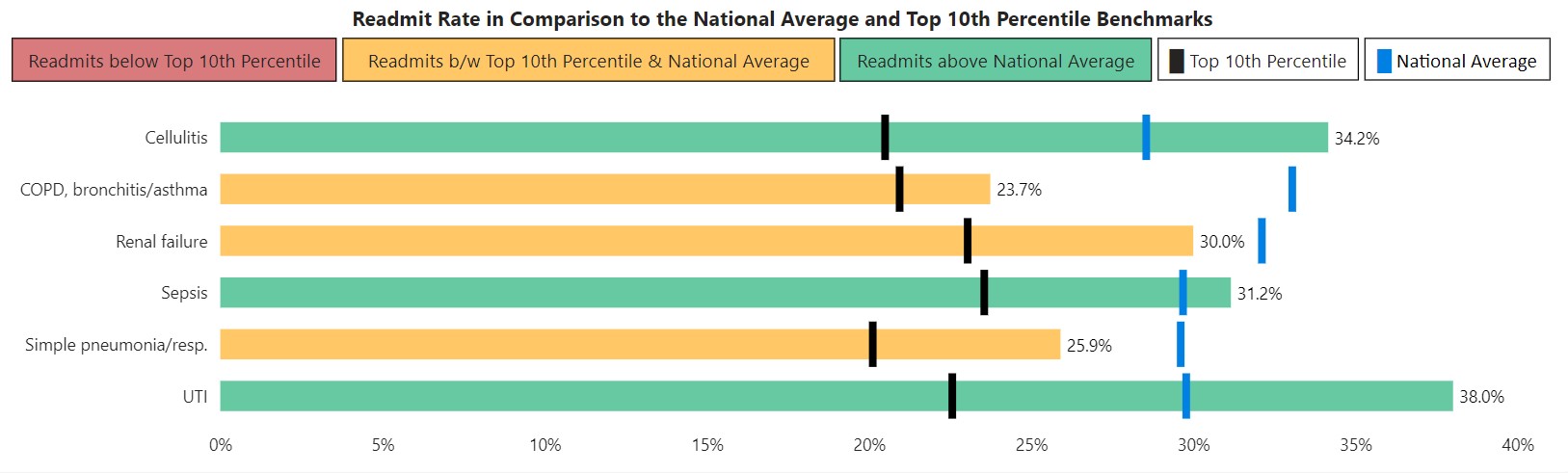
Milliman has developed BPCI-A top 10th percentile PAC utilization benchmarks that enable providers to understand how their population’s BPCI-A PAC utilization compares to other organizations. These benchmarks are available within Milliman’s ACO Shadow Bundle Reporting Interface, which helps MSSP and ACO REACH participants better understand the details and opportunities within the shadow bundles (as shown in the illustration in Figure 1) CMS is providing for their attributed populations. Note that readmission rates above the national average represent the largest opportunity for improvement and are shown in green. Conversely, readmission rates below the top 10th percentile represent the highest performance and a limited opportunity for improvement. They are shown in red.
Figure 1: Readmit rates in comparison to national average and top 10th percentile benchmarks
Consider performance data to help inform specialist referral decisions
Shadow bundles will provide ACOs with hospital performance insights that ACOs may not have access to historically. This data can supplement existing referral decisions by providing ACOs with a perspective on provider cost and utilization performance. ACOs will have performance information available by clinical episode and provider, which they can leverage to optimize referral patterns based on an individual patient’s needs and conditions. ACOs can estimate the impact of referral decisions by comparing the average risk-adjusted episodic cost differences by provider. For example, Figure 2 illustrates the episodic costs for a clinical episode for two providers within an ACO.
Figure 2: Average risk-adjusted episode allowed
As you can see in this example, the anchor spend is higher for Provider B, while the PAC spend is higher for Provider A, resulting in a higher cost of a clinical episode at Provider A. At first glance, one might expect that the ACO should direct care to Provider B over Provider A. However, it is important to take into account other factors, including unit cost differences, each provider’s quality scores, care coordination, patient satisfaction, and volume (e.g., how far is the provider from the patient). Of note, “N” represents the total number of episodes attributed to each provider.
Develop integrated partnerships with high-performing hospitals
Shadow bundles data may also help MSSP and ACO REACH participants make informed decisions on potential hospital system partnerships. Partnerships between ACOs and hospital systems may enable shared goals of patient volume growth, coordinated care, and success in alternative payment models (APMs). Additionally, shadow bundles could be used as a basis to structure risk arrangements between ACOs and hospital systems to improve the cost and quality of care of an ACO’s patient population.
Hospital performance-based negotiations with payers
For ACOs that are part of a hospital system, Medicare FFS shadow bundles could be used as a pathway to gain leverage in their contract negotiations with Medicare Advantage and commercial payers. Hospitals can demonstrate their cost-effectiveness not only in the acute setting, but also in the 90 days post-discharge as leverage in negotiations with payers. Hospitals may also consider structuring value-based payment arrangements with payers leveraging the shadow bundles methodology. Some Medicare Advantage and commercial payers have already started leveraging these types of models to require hospitals to earn future reimbursement rate increases based on performance.
Do shadow bundles represent comprehensive specialist performance?
The shadow bundles that CMS is planning to provide to MSSP and ACO REACH participants are extremely valuable data that can be leveraged to further optimize referral patterns and specialty networks, as well as to identify opportunities to reduce total cost of care. However, given that total cost of care risk in these models extends beyond the episodic care captured within shadow bundles, this data may not provide comprehensive information on specialist performance. A more comprehensive view of specialist performance may include:
1. Beneficiaries that did not experience an acute event (admission or surgery)
As BPCI-A episodes only capture around 23% of Medicare Parts A and B spending, a large volume of beneficiary care will not be captured in the shadow bundles. For example, a specialist who proactively manages their patients’ conditions, which prevents them from seeking emergency or inpatient care, generates significant cost savings that would not be seen in the shadow bundles because the specialists’ patients would not trigger any shadow bundles. Evaluating specialist performance, including all of their patients’ experiences, will provide a more complete picture and lead to better insights into overall performance.
2. Surgeries performed outpatient or at ambulatory surgical centers (ASCs)
Evaluating a surgeon’s performance based solely on inpatient surgeries may miss a significant portion of the surgeries. Many surgeries are now performed in an outpatient setting or at ambulatory surgical centers (ASCs), both of which are intended to be lower in cost compared to equivalent inpatient locations for a given patient. In some specialties, most surgeries are performed outpatient, and the surgeries that are required to be performed inpatient may be due to an emergency or a very high-risk patient. These scenarios are low-frequency and can be difficult to appropriately risk-adjust. Episode definitions that anchor on surgeries performed in all settings will more accurately represent a surgeon’s performance.
3. Expenditures across the entire patient journey of a disease or surgery
While shadow bundles can provide insights into expenditures occurring 90 days post-discharge or -surgery, a significant proportion of the patient journey of care may be missing. Evaluating specialist performance inclusive of care that occurs prior to the hospital admission or surgery would give a more comprehensive picture of the patient journey and costs incurred. For example, the number of tests or radiology services performed prior to a surgery, the site of care in which these services were performed, or leveraging physical therapy or other lower-cost alternatives to avoid the surgery altogether could all contribute to how efficient and effective a specialist is at managing care. Accounting for these efficiencies when evaluating specialist performance can lead to significant cost improvements and more accurate benchmarking.
4. Evaluating performance based only on claims specific to the condition the specialist is managing
While management of chronic conditions or outcomes related to surgeries may have an impact on a member’s total cost of care and outcomes, specialists may not always be responsible for care unrelated to the condition they are managing. Specialists may push back on a methodology that includes care that they have no influence over. An ideal evaluation of specialist performance would focus solely on the care they are able to manage and influence. In some cases, this may be on total cost of care but, in many cases, it should only be care specific to the condition or surgery they are managing.
To better understand how specialty care contributes to the total cost of care, ACOs may want to leverage specialist performance benchmarking that accounts for at least some of the above items and leverages a more comprehensive dataset (e.g., 100% Medicare FFS dataset) as found in Milliman’s ACO Builder Specialist Explorer.
Conclusion
An organization that has enrolled in both an ACO and bundled payment program often manages them separately and might not be able to fully realize opportunities and synergies that can be leveraged across the programs. Examining episodic data within an ACO’s data can produce better alignment, increased awareness, and potentially broader opportunities for shared savings.
Data alone will not change behavior or solve any inherent issues within a condition, a health system, or an ACO. Understanding the data, uncovering possible opportunities, and firmly committing to instituting change are all necessary components of success. Milliman has extensive subject matter expertise and data-driven tools (including specialist performance benchmarking modules) for both ACO and bundled payment programs to help highlight an organization’s ability to better align with specialists.
1 CMMI survey of ACO Reach and Medicare Shared Savings Program ACOs in spring 2023.
2 Bazell, C., Alston, M., Pelizzari, P.M., & Sweatman, B.A. (March 27, 2023). What Are Bundled Payments and How Can They Be Used by Healthcare Organizations? Retrieved February 11, 2024, from https://www.milliman.com/en/insight/what-are-bundled-payments-and-how-can-they-be-used-by-healthcare-organizations.
