The foundation of the AHEAD model is primary care-focused multi-payer (including Medicare, Medicaid, and commercial) alignment among the participating state agencies and their provider communities. AHEAD intends to reduce healthcare costs while improving and reducing disparity in population health outcomes.
Timeline
- On November 16, CMS released the first of two Notice of Funding Opportunity (NOFO) application periods.
- Participants are divided into three cohorts (Cohorts 1-3) varying by “readiness” to implement. Application due date, duration of pre-implementation period, and first performance year start date vary by cohort.
- A pre-implementation period, which is used to plan care redesign, is either 18 months (Cohort 1), 24 months (Cohort 3), or 30 months (Cohort 2), depending on the cohort.
- The first performance year (PY) is either 2026 (for Cohort 1) or 2027 (for Cohorts 2 and 3) with subsequent performance years continuing through 2034.
Figure 1 summarizes the differences in the cohorts and timelines.
AHEAD fast facts
- AHEAD applicants are state agencies (e.g., state Medicaid agency, state public health agency, state insurance agency, or other entity with rate-setting or budget authority).
- CMS will provide cooperative agreement funding for up to $12 million dollars (for up to six years) to eight applicants or “award recipients.” This can be used for planning and implementation activities. Attached to this are various model milestones for continued funding support.
- The provider community aligning with the state agency and private payers includes hospitals and primary care practices. Award recipients will be required to recruit hospitals and primary care practices to participate, specifically at least one commercial payer needs to participate in hospital global budgets by the start of PY2.
- AHEAD is scheduled to operate for a total of 11 years, from 2024 through 2034. Performance years (PYs) will begin either in January 2026 or January 2027, depending on the cohort.
- Hospital providers may join the AHEAD Model in any PY. However, only hospitals joining in PY1 or PY2 will be eligible to receive an up-front 1% adjustment to their Medicare fee-for-service (FFS) global budgets to invest in care transformation activities. (Refer to ”Transformational Incentive Adjustment” in the NOFO for more details.)
Figure 1: Timelines1
| Cohort | Letter of Intent | Application Due | Award Notice | Duration of Pre-Implementation Period |
First Performance Year (PY1) |
Last PY |
|---|---|---|---|---|---|---|
| 1 | Feb 5, 2024 | Mar 18, 2024 | May 2024 | 18 months | 2026 | 2034 |
| 2 | 18 months | 2027 | 2034 | |||
| 3 | Jul 26, 2024 | Aug 12, 2024 | Oct 2024 | 24 months | 2027 | 2034 |
AHEAD model overview
Background
AHEAD is a voluntary multi-payer total cost of care (TCOC) model. CMS defines a TCOC model2 as one in which a designated entity, in this case a state agency, takes on the financial responsibility and administrative oversight for managing the total healthcare costs for a given population. While AHEAD uses TCOC growth targets to create statewide accountability for limiting cost growth (across all payers), the AHEAD model framework emphasizes hospital global budgets and primary care.
AHEAD is built on cooperative agreement of multi-payer alignment, with the “state Medicaid and Health agencies” taking a lead role in bringing together stakeholders and overseeing implementation across Medicare FFS, Medicaid, and Commercial lines of business. AHEAD’s model “components” drive the cost savings, while the model “strategies” look to achieve objectives of maintaining or even improving the quality of care provided to benefit the community. Furthermore, a key strategy of AHEAD is to improve health equity by supporting underserved communities.
Achieving success in AHEAD
Broad components of the AHEAD model have been outlined by CMS3 and detailed in the NOFO.4 Given that the accountability targets (e.g., global hospital budget) are based on Medicare FFS metrics, the AHEAD model may seem to focus on Medicare FFS, but alignment with Medicaid and commercial payers is just as critical to achieving success in the model. Drawing from similar risk models and the available information of the AHEAD model, state participation in AHEAD must meet the “State Accountability Targets” and goals underlying the model “Components” and “Strategies” described below.5 Furthermore, to achieve alignment with the Medicaid and commercial markets, each of these areas must specify how Medicaid and private payers will participate and how the results will be measured.
Targets and components
- Statewide or substate accountability targets underlie each model component and strategy. CMS defines the financial targets for Medicare FFS and the states must extend them to all of the payers (i.e., Medicare FFS, private payer, Medicaid).
- Cooperative agreement funding is tied to defining the model governance structure and quantifying the goal and targets that the state is accountable to achieve as an AHEAD award recipient.
- Hospital global budgets provide hospitals with a prospective fixed amount of revenue for the upcoming year for a specific patient population. Contributions by payer will depend on historical unit price, negotiated or legislated changes in unit price, and expected utilization, with adjustments for quality, site of care shifts, and budget discounts.
- Primary care investment is foundational to high-performing health systems and improving health outcomes for the community and lowering cost.6 Similar to hospital budgets, contributions by payer will depend on expected utilization, historical unit price, and negotiated or legislated changes in unit price. The funding mechanism may be a mix of fixed payments (e.g., capitation and/or incentive payments) and per service payments to balance funding based on work performed and care transformation investment. CMS is hoping to achieve specific targets for Medicare FFS (approximately 6%-7%) and all-payer (either set by local policy or more national standards such as Medicare FFS).
Strategies
CMS expects that state agencies can use policy and regulatory levers (e.g., Medicaid policy, commercial market regulation, provider rate setting, incentives, and penalties for exceeding all-payer TCOC spending targets, etc.) to promote multi-payer alignment and manage expenditure growth. In addition, they can motivate and influence stakeholders because states have historically been the center point for the local governments, community, providers, and local nonprofit organizations.
States have flexibility in how they implement these strategies and measure success. However, CMS requires states to develop targets, measurement process, and report results for each area.
- Population health: Most broadly, defining how the stakeholders will align and drive changes in the areas of prevention, wellness, and behavioral health as well as incentivizing the appropriate services.
- Healthcare quality and utilization: To ensure provider care continues while costs are being reduced, quality and utilization measures would be selected based on appropriateness and alignment with goals of stakeholders (i.e., state agency, hospitals, primary care practices), while balancing administrative costs and ensuring alignment across models and payers.
- Behavioral health (BH): In addition to the component of behavioral health integration, states should, from a strategic point, consider how the model aligns with their specific needs and ongoing initiatives in behavioral health. This includes a focus on the network infrastructure, reporting of quality metrics, delivery of care, and helping those with complex BH-related conditions.
- Health equity advancement: This will require specific budgets, funding, and quality measurements oriented toward a state agency’s health equity goals. CMS defines health equity as “the attainment of the highest level of health for all people, where everyone has a fair and just opportunity to attain their optimal health regardless of race, ethnicity, disability, sexual orientation, gender identity, socioeconomic status, geography, preferred language, or other factors that affect access to care and health outcomes.”7 Alignment on the health equity goals and associated measures should be determined up-front, so the hospital budget, primary care funding, and quality measurement approach and incentives are consistent across payers and stakeholders. The AHEAD model frames a statewide health equity plan (State HEP), or, at the provider level, a Hospital HEP.
- Behavioral health (BH) integration: This includes how hospital budgets, primary care funding, and total cost of care trend targets will support the BH services.
- State TCOC growth targets: TCOC targets are designed to ensure changes in hospital and primary care funding rebalance healthcare spending, rather than increase overall spending. Participants are expected to limit Medicare FFS spending growth relative to the “counterfactual” (i.e., expected cost growth in the absence of AHEAD participation). Similarly all-payer TCOC growth targets must be established and should incorporate payer-specific factors that affect total cost of care trends (e.g., population aging and health status changes).
- Multi-payer (or all-payer) alignment: One key strategy is to bring multiple otherwise distinct markets (Medicaid, commercial, Medicare) and stakeholders (CMS, payers, providers) together to share in common goals including reduced costs and improved quality in the healthcare. By combining these payers in a single model, there is greater diversification of risk, influence over the market, and reductions in the disparities naturally borne within each market, while also aligning incentives and creating operational efficiencies.
A brief history of TCOC
We have seen multiple past CMS risk-based models attempting to align incentives across payers—many of which include global hospital budget components and total cost of care trend targets. Figure 2 shows a basic comparison of key components of each model. For more details, please see the respective source.
- Vermont All-Payer ACO Model
- Pennsylvania Rural Health Model
- Maryland Total Cost of Care Model
- CMS CHART Model
Vermont All-Payer Model
The Vermont All-Payer Model spans across all major payers in the state, designed to incentivize broad delivery system transformation to reduce statewide spending and improve population health outcomes. The model began in 2017 and is scheduled to conclude at the end of 2024. To date, the model has seen notable decreases in acute and specialty care spending, as well as increases in primary care visits. However, the model has not achieved the intended level of engagement from payers and providers, which has kept the major payment method as FFS.8
Pennsylvania Rural Health Model
To maintain access to essential healthcare services in rural communities, the Pennsylvania Rural Health Model (PARHM) is testing the impact of hospital global budgets and care delivery transformation. The model began in 2019 and is scheduled to complete at the end of 2024. Participating hospitals experienced improvements in financial sustainability metrics following the introduction of the model. However, hospitals mentioned that the global budget was not sufficient to fund hospital care delivery transformation, though it did accelerate their community engagement activities.9
Figure 2: Multi-payer TCOC program comparison
| Model Components | AHEAD | CHART | VT | MD TCOC | PA |
|---|---|---|---|---|---|
| Model Status Performance Years | Open 2023-2027 | Withdrawn 2022-2023 | Completed 2017-2022 | Ongoing 2019-2026 | Ongoing 2019-2024 |
| Global Hospital Budget | Y | Y | N | Y | Y |
| Primary Care Funding Target | Y | N | N | N | N |
| Behavioral Health Integration | Y | Y | N | N | Y |
| Quality Measurements | Y | Y | Y | Y | Y |
| Total Cost of Care | Y | Y | Y | Y | N |
| Multipayer alignment | Y | Y | Y | Y | Y |
Maryland Total Cost of Care Model
As the first model to hold a state fully at risk for the total cost of care for Medicare beneficiaries, the Maryland TCOC Model builds upon its predecessor, the Maryland All-Payer Model, which had set a limit on per capita hospital expenditures in the state. The Maryland TCOC Model began in 2019 and concludes at the end of 2026. Particularly notable is the participation of most of the hospitals in Maryland. Figure 3 illustrates the improvement in performance of the TCOC model on top of the all-payer model. Both models led to significant improvement in spending, service use, and quality of healthcare in Maryland.10 Particularly notable was the reduction in hospital admissions and preventable admissions.
Figure 3: Maryland results from 2017-2021
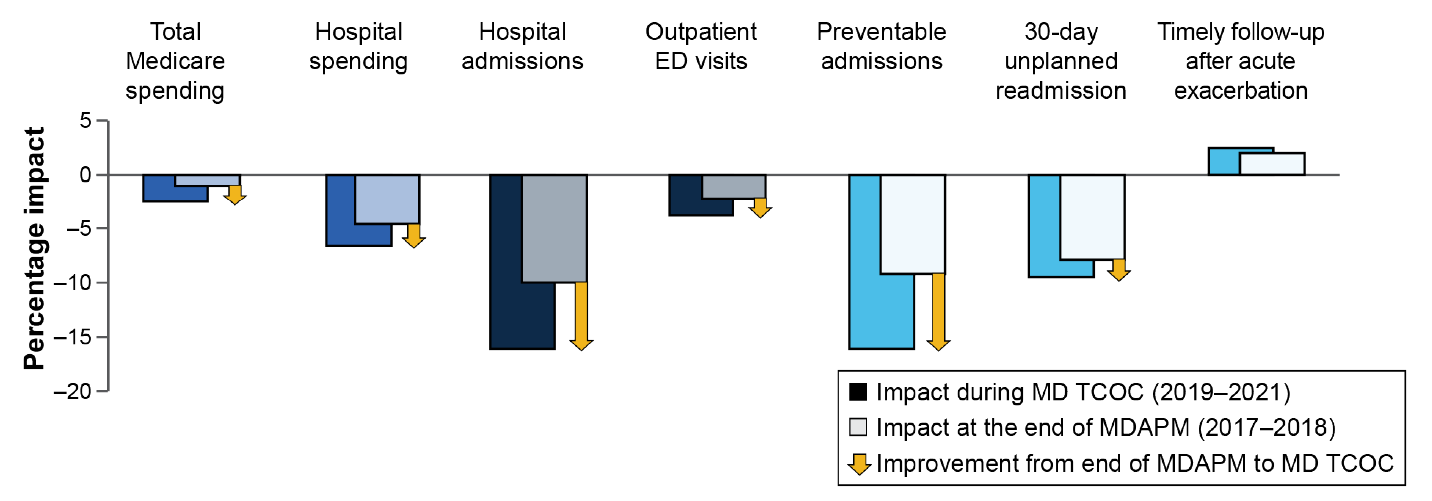
Source: Maryland TCOC Model, CMS Findings at a Glance Report.
CHART Model
In 2020, CMS had announced Community Health Access and Rural Transformation (CHART) Model11 to go live in 2022. The focus of this model was to help underserved communities in rural locations. In September 2021, the model selected and awarded the agreement to lead organizations (i.e., the oversight body) in Alabama, South Dakota, Texas, and Washington state. The next step was for these lead organizations to develop and implement a healthcare redesign model. However, in September 2023, CMS released this statement, which indicated the termination of the model:
Based on feedback received from Model stakeholders, as well as a lack of hospital participation, the CHART Model will end early on September 30, 2023
CMS specifically acknowledges and intends to carry forward lessons learned from its experience from CHART, including financial methodologies, community led transformation, and health equity, to bolster the AHEAD model.
What do I do now? Important application information for state agencies
CMS has provided high-level guidance of the AHEAD model and released the first two application periods, for Cohorts 1 and 2. Interested parties can take the following actions.
- Review available resources provided by CMS at https://www.cms.gov/priorities/innovation/innovation-models/ahead.
- Review the NOFO and application requirements. Specifically, pay close attention to the “Budget Narrative” and “Project Narrative.” Briefly, the Project Narrative focuses on the ”what” and ”how” of the project, detailing the goals, objectives, strategies, and plans. On the other hand, the Budget Narrative focuses on the ”how much,” providing a detailed breakdown of the project costs and a plan for financial sustainability. These are detailed in the NOFO in sections E. Application Review Information. See https://www.grants.gov/search-results-detail/349644.
- Understand the purposes of the various agreements: Cooperative Agreement (an outcome of the NOFO), State Agreement (model terms between state agency and CMS), and Participation Agreements (state agency terms with providers).
- Understand the potential overlaps of primary care providers participating in AHEAD versus other CMS or Center for Medicare and Medicaid Innovation (CMMI) programs. Primary care providers can participate in AHEAD and risk-based programs like Accountable Care Organizations Realizing Equity, Access, and Community Health (ACO REACH) or the Medicare Shared Savings Program (MSSP). However, providers cannot participate in both AHEAD and primary care programs like Primary Care First (PCF) or Making Primary Care (MCP). In addition, hospitals participating in episode-based programs will be evaluated on a case-by-case basis.
- Perform analytics with relevant measures by market including historical TCOC growth, share of primary care investment for Medicare (CMS estimates targets will be 6%-7% of TCOC), as well as look-back analyses to understand the potential impacts of proposed models.
- Begin identifying and consider engaging stakeholders in discussions. One of the shortcomings in CHART was provider participation. Understanding provider needs seems critical to get the AHEAD model off the ground.
- Applicants should submit a letter of intent (LOI) by either February 5, 2024 (for Cohorts 1 and 2), or July 26, 2024 (for Cohort 3).
Closing thoughts
The AHEAD model is a new TCOC initiative by CMS that aims to reduce healthcare costs and improve health equity across populations. The model’s primary financial mechanisms are TCOC growth targets, hospital budgets, and primary care investment. The model is expected to move further along the development stage than CHART, and in the footsteps of the (to date) successful TCOC models in Maryland, Pennsylvania, and Vermont.
While the AHEAD model provides states with a large amount of flexibility in terms of how it is implemented, success or failure will largely be based on the degree to which states are able to engage and align providers and payers and drive total cost of care reductions with at-risk populations, all while working within the limited resources (up to $12M over 6 years) provided.
AHEAD is set to operate from 2024 through 2034 and offers a unique opportunity for state agencies with strong community partnerships to share the risk across Medicare, Medicaid, and commercial markets. The model's success will hinge on meeting CMS’s Medicare FFS targets, alignment with Medicaid and private payers, and the interactions of various components such as hospital global budgets, primary care funding, quality measures, health equity advancement, behavioral health integration, and TCOC growth management. With the release of the NOFO for Cohort 1 and Cohort 2, interested parties can now prepare by scheduling stakeholder discussions and closely following the timeline provided by CMS.
1 CMS (September 5, 2023). States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model. Press release. Retrieved December 12, 2023, from https://www.cms.gov/priorities/innovation/innovation-models/ahead.
2 CMS. Total Cost of Care and Hospital Global Budgets. Retrieved December 12, 2023, from https://www.cms.gov/priorities/innovation/key-concept/total-cost-care-and-hospital-global-budgets.
3 CMS (September 5, 2023), op cit.
4 CMS. States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model. Grant Notice. Retrieved December 12, 2023, from https://www.grants.gov/search-results-detail/349644.
6 CMS (September 5, 2023), op cit.
7 CMS, AHEAD Model, Grant Notice, op cit.
8 CMS. Vermont All-Payer Model. Findings at a Glance. Retrieved December 12, 2023, from https://www.cms.gov/priorities/innovation/data-and-reports/2023/vtapm-3rd-eval-report-aag.
9 CMS. Pennsylvania Rural Health Model (PARHM). Findings at a Glance. Retrieved December 12, 2023, from https://www.cms.gov/priorities/innovation/data-and-reports/2023/parhm-ar3-aag.
10 CMS. Maryland Total Cost of Care (MD TCOC) Model. Findings at a Glance. Retrieved November 6, 2023, from https://www.cms.gov/priorities/innovation/data-and-reports/2022/md-tcoc-qor2-aag.
11 CMS. CHART Model. Retrieved December 12, 2023, from https://www.cms.gov/priorities/innovation/innovation-models/chart-model.